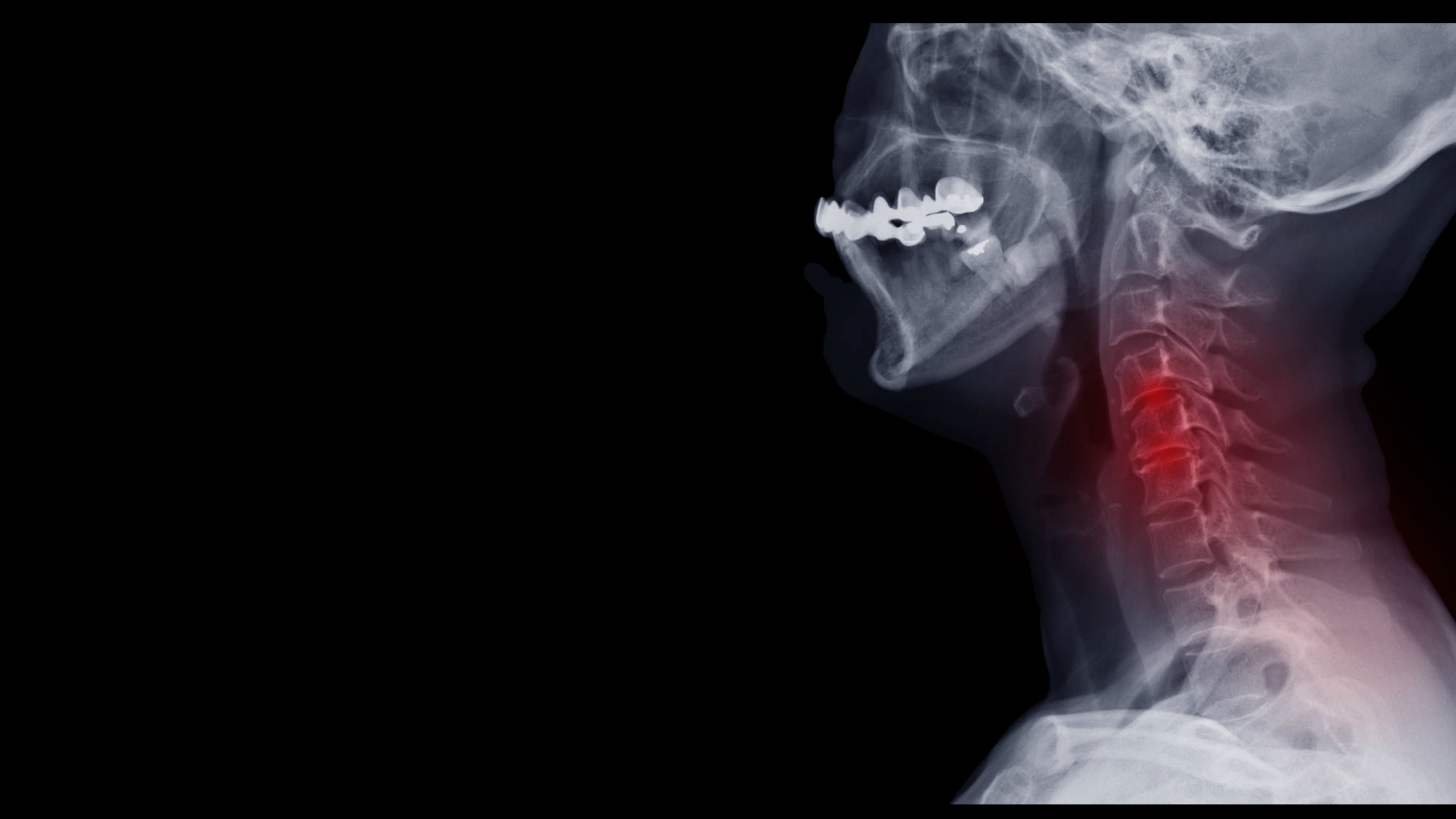
While the only true way to determine whether or not you need a cervical spinal fusion is to consult with a neurosurgeon, there are some signs that you can watch out for that may help you determine when it’s time to set up that doctor’s appointment. One of the biggest tell-tale signs that you may need surgical intervention for your neck pain is symptoms caused by progressive nerve damage. Damage in the cervical spine, often referred to as cervical radiculopathy, can cause problems with not only your neck but can radiate pain throughout your arm as well. Some symptoms of nerve damage include sharp, burning, or aching pain that may radiate outwards, tingling, pins and needles sensations, and muscle weakness in the affected area. Neck pain can also be a sign that there is pressure on your spinal cord, which can cause other problems if not dealt with properly.
Signs You Might Need Cervical Spinal Fusion
Another sign you may need to consider cervical spinal fusion is if more conservation treatment options did not help your symptoms subside. The amount of time a person should explore non-surgical options depends on the individual’s pain tolerance, their personal interest in pursuing surgery, and their doctor’s expert opinion. Once your neck pain is determined to be chronic and resistant to conservative treatments, it is likely that your doctor will discuss the possibility of a cervical spinal fusion. If your doctor anticipates that your symptoms will worsen and cause more problems for you down the line, they may encourage you to explore the surgical route.
Understanding Cervical Spinal Fusion Surgery
There are many different types of cervical spine surgeries that one can receive, and one of these is cervical spinal fusion. When your spine surgeon recommends cervical spine fusion surgery, the actual surgery they are usually referring to is an anterior cervical discectomy and fusion (ACDF) surgery (Mayo Clinic), although this surgery can be performed posteriorly as well. Studies have shown that regardless of if the surgery is performed anteriorly or posteriorly (NCBI), there is no significant difference in recovery. This surgery can be performed to alleviate symptoms causes by a cervical herniated disc, cervical degenerative disc disease, cervical spine stenosis and any cervical spondylotic myelopathy.
When someone develops degenerative disc disease, it causes the discs to dry out. When these discs dry out, tears in the disc annulus will begin to form which can allow the gel-filled nucleus material to escape and compress the spinal cord. This compression of the spinal cord can cause numbness and weakness. In addition, bone spurs may develop, possibly leading to the narrowing of the nerve root canal. Then, the pinched nerve will become both swollen and painful.
An anterior cervical discectomy and fusion is a surgery that is performed to remove a degenerative or herniated disc in the neck. This is done by making an incision in the throat area in order to reach and remove the disc. The doctor will then move aside the neck muscles, trachea, and esophagus so that the disc and bony vertebrae can be reached without obstructions. Doctors usually opt for the anterior version of this surgery because the disc can be reached without disturbing the spinal cord, spinal nerves, and neck muscles. Depending on your specific symptoms, your doctor may opt for either a single-level discectomy or a multi-level discectomy. Once the disc is removed, a graft is inserted into the space between the bony vertebrae. This is done in order to prevent the vertebrae from collapsing and rubbing together.
Types of Bone Grafts Used in Cervical Spinal Fusion
The spacer bone graft used to fill the open disc space can come from many different places, each having their own advantages and disadvantages. An autograft bone is a bone that comes from your own body. Your surgeon will take your own bone cells from your hip’s iliac crest. The advantage of this type of graft is that it has a higher rate of successful fusion since it is composed of bone-growing cells and proteins. The downside of an autograft bone is the pain you may feel in your hipbone post-surgery. An allograft bone is a bone that comes from a cadaver. While this type of graft lacks bone-growing cells and proteins, it is a readily available option and eliminates having to harvest bone from your hip. Another type of graft is a man-made one known as a bone graft substitute. These grafts are usually made from plastic, ceramic, or bioresorbable compounds. Also referred to as cages, both these and allografts are packed with shavings of living bone tissue taken from your spine during surgery.
The bone graft serves as a bridge between the vertebrae above and below the disc in question in order to complete the spinal fusion part of the surgery. Your surgeon will fix the bone graft and vertebrae in place with the use of metal plates and screws. Post-surgery, your body will start its natural healing process and new bone cells will begin to grow around the graft. In 3 to 6 months, the bone graft should have joined the vertebrae and formed a solid piece of bone.
Preparing for Cervical Spinal Fusion Surgery
To determine whether or not surgical intervention is the correct approach to treat your neck pain, you will need to consult either a neurosurgeon or orthopedic surgeon. You will need to sign consent forms and fill out paperwork so that your doctor knows and understands your medical history (bleeding history, anesthesia reactions, prior surgeries, medications, etc.). Your doctor may also request presurgical tests like blood tests, x-rays, or other tests in order to make sure you are fit for surgery.
A week before your scheduled surgery date, you should cease taking all non-steroidal anti-inflammatory medicines and blood thinners. You should also stop drinking alcohol and using nicotine to avoid any healing and bleeding problems. The most important thing you can do before cervical spinal surgery is the stop using any tobacco, which includes cigarettes, vaping, pipes, dip, cigars, and any other form of tobacco and nicotine consumption. Nicotine actually prevents bone growth and significantly impacts whether or not your fusion is successful. Studies have shown that spinal fusion fails in 40% of smokers compared to only 8% in non-smokers.
Recovery and Post-operative Care
After you go through cervical spinal fusion, you will find yourself in the postoperative recovery area. A nurse will monitor your vitals, which includes your blood pressure, heart rate, and respiration. Most patients are sent home the same day after surgery, but if you are experiencing difficulty breathing and unstable blood pressure, they may keep you overnight. For two weeks after surgery, there are many rules you need to follow in order to ensure your cervical spinal fusion is as successful as possible. You should avoid bending or twisting your neck, don’t lift anything heavier than 5 pounds, avoid strenuous activity (yes, this also includes sex!), don’t smoke or use any products containing nicotine, don’t drive, and don’t drink alcohol.
You will most likely have a follow-up appointment with your surgeon 2 weeks after surgery, although recovery time typically lasts for 4-6 weeks. At some point, x-rays may be taken to ensure that the fusion is working, which will determine if your doctor clears you for work. Sometimes, your doctor will ask you to wear a cervical brace or collar to provide your neck with support and limit its motion. Once your neck has healed, your doctor will most likely prescribe you with physical therapy, as neck pain recurrences are common and since the goal of this surgery is to get rid of it, it is essential to take care of your neck. To avoid neck pain returning, you should learn proper lifting techniques, good posture, adopt an appropriate exercise regime, invest in an ergonomic work area, maintain a healthy weight, stay positive, and stay away from smoking.
Results and Potential Complications
For patients experiencing arm pain due to neck issues, anterior cervical discectomy and fusion surgery (Pub Med) is successful in relieving pain in 92-100% of patients, although this pain can persist for weeks or months after surgery. When it comes to neck pain, about 73-83% of patients found relief from this surgery. These results are also largely dependent on how you take care of your fusion post-surgery.
While this surgery is usually very successful, no surgery comes without risks. Some anterior cervical discectomy and fusion surgery complications can include hoarseness and swallowing difficulties, failure of the vertebrae fusing, hardware fracture, bone graft migration, adjacent segment disease, and nerve damage or persistent pain.
Although these complications may sound scary, studies assessing the long-term clinical outcomes of anterior cervical discectomy and fusion surgery (Pub Med) saw significant improvements. The outcomes of this study were in no way related to age, gender, number of levels treated, and preexisting degeneration of the adjacent levels. The study found that the use of narcotic pain kills decreased a lot and neurological deficits almost all completely resolved. The patients self-reported a success range from 85-95% after 10 years, showing that this surgery is a great option for those suffering with cervical spine issues that just want to get back to their normal lives.