Vasectomy, often chosen by men seeking a permanent form of birth control, involves a minor surgical procedure that prevents sperm from entering the semen. Annually, about 600,000 men in the U.S. opt for this procedure, valuing its effectiveness and simplicity. However, life circumstances such as new partnerships or the desire for more children can lead some to reconsider their decision. Vasectomy reversal emerges as a beacon of hope for these individuals, offering a path back to fertility. This surgical endeavor, while complex, has been refined over the years to increase its success rate and minimize associated risks.
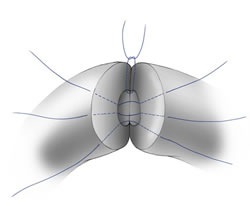
Vasectomy reversal is a testament to the advancements in medical technology and surgical precision. The procedure meticulously reconnects the vas deferens, the tubes severed during a vasectomy, to allow sperm to once again mix with semen. Performed with the aid of a high-powered surgical microscope, this operation requires a skilled hand and several hours of focused effort. Despite its complexity, the procedure is typically done on an outpatient basis, allowing patients to return home the same day. The decision to undergo a reversal is significant, prompting many to weigh the potential for restored fertility against the challenges and risks involved.
Understanding Vasectomy Reversal
A vasectomy reversal is a complex and delicate surgery that aims to reconnect the vas deferens, the tubes that were cut during a vasectomy, to allow sperm to enter the semen once again. This procedure is performed under a microscope with high precision to ensure the best possible outcome. The surgery can take between 2 to 3 hours and is usually done on an outpatient basis, meaning the patient can go home the same day. The complexity of the surgery increases with the time elapsed since the original vasectomy, as blockages can form and some men may develop antibodies to their own sperm.
Success Rates of Vasectomy Reversal
The success of a vasectomy reversal largely depends on the time that has passed since the original vasectomy. Generally, reversals performed within the first 10 years have a higher success rate, with more than half of these cases resulting in pregnancy. Beyond the 10-year mark, the success rate drops to about 30%. The skill and experience of the surgeon play a crucial role in the procedure’s success, making it essential for patients to choose a specialist with a proven track record in performing vasectomy reversals.
Risks Associated with Vasectomy Reversal
As with any surgical procedure, vasectomy reversal carries certain risks, including infection at the surgery site, fluid buildup in the scrotum, and injury to arteries or nerves in the scrotum. These risks underscore the importance of selecting an experienced surgeon and adhering to post-operative care instructions to minimize complications.
Preparing for a Vasectomy Reversal
Before undergoing a vasectomy reversal, it’s important for the patient to undergo evaluations to confirm fertility prior to the original vasectomy and to check for the presence of sperm antibodies in the semen. The presence of sperm antibodies post-surgery can significantly reduce the chances of achieving pregnancy.
The Importance of In-Home Care After Vasectomy Reversal
Recovery from vasectomy reversal is a critical period that requires careful management to ensure the best possible outcome. In-home care plays a vital role in this process, encompassing several key aspects:
- Pain Management: Patients will likely experience discomfort and swelling following the procedure. It’s important to follow the surgeon’s instructions regarding pain medication and to apply ice packs as recommended to reduce swelling.
- Activity Restrictions: To promote healing, patients are advised to limit physical activity and avoid lifting heavy objects for a specified period. Rest is crucial in the first few days after surgery.
- Wound Care: Keeping the surgical site clean and dry is essential to prevent infection. Patients should follow their surgeon’s guidelines on how to care for the wound and when it’s safe to shower or bathe.
- Follow-up Appointments: Attending follow-up appointments allows the surgeon to monitor the healing process and address any concerns that may arise. It’s also an opportunity to evaluate the success of the reversal in terms of sperm presence in the semen.
Pathways to Parenthood: Navigating Recovery and Success
The journey toward recovery and the potential restoration of fertility following a vasectomy reversal is marked by careful planning and adherence to post-operative care. The success of this procedure hinges not only on the surgeon’s skill but also on the patient’s commitment to following through with the necessary in-home care measures. Pain management, activity restrictions, and wound care are pivotal components of the recovery process, each playing a crucial role in ensuring a smooth and effective healing period. Moreover, follow-up appointments provide an essential feedback loop, allowing for the monitoring of progress and the adjustment of care plans as needed.
As patients navigate the post-operative landscape, the prospect of achieving pregnancy looms as a beacon of hope. The success rates of vasectomy reversals, while influenced by the time elapsed since the original procedure, offer encouragement to many. With more than half of reversals resulting in pregnancy within the first ten years, the dream of expanding a family becomes tangible. This journey, underscored by the advancements in surgical techniques and the personalized care received both in the hospital and at home, reflects the resilience and determination of those seeking to reverse a once permanent decision. Vasectomy reversal is more than a medical procedure; it’s a pathway to renewed hope and the possibility of new beginnings.