What Is Venous Reflux Disease?
Venous reflux disease (VRD), also known as chronic venous insufficiency (CVI), is a widespread condition that affects millions of adults in the United States. Nearly 40% of Americans experience chronic venous issues. Yet many people don’t recognize the early signs or seek care until symptoms become more severe.
VRD is progressive. If left untreated, it can lead to skin changes, open sores, and lasting discomfort. Fortunately, early treatment and lifestyle adjustments can slow the disease’s progression and ease symptoms. Managing VRD often requires a whole-body approach.
Many people combine medical care with supportive services, such as holistic vein care, to manage the physical condition and support overall well-being. Holistic strategies focus on prevention, lifestyle, and long-term guidance to improve both circulation and quality of life.
Causes and Risk Factors of Venous Reflux Disease
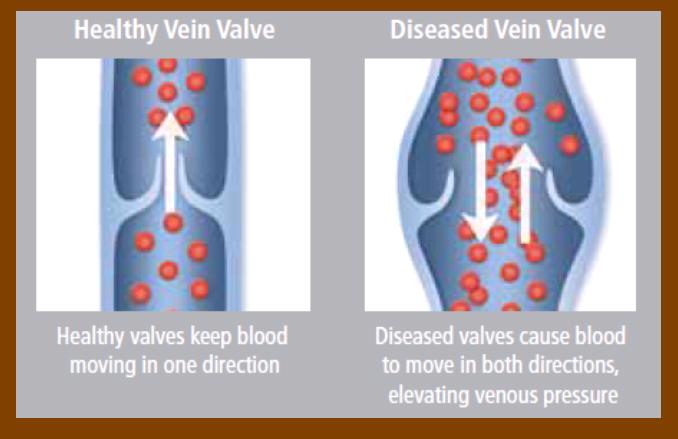
VRD can develop for many reasons, including damage to the veins, genetic traits, and lifestyle factors. Common causes include:
- Damage to vein valves from deep vein thrombosis (DVT)
- Weak or stretched vein walls that interfere with proper valve function
- Being born without certain vein valves
- Blockages in the pelvic or groin veins
Risk factors that raise your likelihood of developing VRD include:
- Family history of vein disease
- Excess weight or obesity
- Pregnancy, especially multiple pregnancies
- Sitting or standing for long periods
- Limited physical activity
- Being over age 50
- Smoking or tobacco use
- High blood pressure
- Past leg injuries or surgeries
Knowing your risk helps you make informed decisions. Many people use this insight to build a long-term plan through holistic wellness centers focused on vein health.
Signs and Symptoms of Venous Reflux Disease
Symptoms of VRD often begin gradually and worsen over time if not addressed. Common signs include:
- Tired, heavy, or achy legs
- Swelling in the lower legs or ankles
- Burning or tingling sensations
- Night cramps in the legs
- Restless legs
- Darkened or discolored skin around the ankles
- Itchy or flaky skin
- Enlarged, twisted varicose veins
- Thickened or firm skin
- Open sores or ulcers, typically near the ankles
These symptoms can worsen after long periods of sitting or standing. Treating VRD early can reduce discomfort and lower the risk of complications.
How Is Venous Reflux Disease Diagnosed?
To diagnose VRD, healthcare providers start with a physical exam and a review of your medical history and symptoms. They look for visible signs like swelling, skin changes, or varicose veins and may ask about pain, cramping, or skin irritation.
A noninvasive imaging test called a venous duplex ultrasound is commonly used to see how well blood flows through the leg veins. It helps identify where blood is backing up or valves are malfunctioning. Other imaging tools like MRI or CT scans may be used in some cases to assess deeper vein structures and rule out other causes.
A clear diagnosis helps shape a customized treatment plan focused on your condition and overall health goals.
Treatment Options for Venous Reflux Disease
Treatment for VRD focuses on restoring healthy blood flow, easing symptoms, and preventing the condition from worsening. Common options include:
- Lifestyle changes – Regular exercise, leg elevation, weight management, and limiting prolonged standing or sitting.
- Compression therapy – Special stockings that apply pressure to improve circulation and reduce swelling.
- Medications – Antibiotics may treat infections, while anticoagulants may be used to prevent clots in certain cases.
- Sclerotherapy – A minimally invasive treatment that involves injecting a solution into affected veins to close them off.
- Endovenous ablation – A procedure that uses heat to seal malfunctioning veins.
- Surgery – Reserved for more severe cases, where problematic veins may be removed or bypassed.
- Holistic approaches – Many individuals turn to integrative therapies such as massage, nutrition support, and wellness coaching to manage symptoms and support whole-body health.
Treatment plans vary based on your needs, symptoms, and overall condition.
Complications of Untreated Venous Reflux Disease
When venous reflux disease goes untreated, it can lead to serious complications. As pressure builds in the veins, skin may become damaged or discolored. Open sores near the ankles, known as venous ulcers, may develop and take a long time to heal.
Other risks include skin infections like cellulitis, chronic pain, and long-term leg swelling. These complications can reduce mobility and impact daily life. Timely diagnosis and consistent care are key to avoiding these outcomes.
Prevention and Long-Term Management
While not always preventable, VRD can often be managed or slowed with everyday habits. Small lifestyle changes can have a big impact.
Exercise regularly to strengthen your leg muscles and support blood flow. Take walking breaks if your job requires long hours sitting or standing. Avoid tight clothing that restricts circulation.
Maintaining a healthy weight reduces strain on your veins, while eating a balanced, heart-healthy diet helps manage swelling and blood pressure. Quitting smoking also supports both vascular and heart health.
If you’re living with VRD, ongoing care is essential. Wear compression stockings as directed, elevate your legs when possible, and follow a consistent skincare routine to protect sensitive areas. Many people also benefit from wellness-based support that complements medical care.
When to Seek Medical or Holistic Care
Early signs of VRD are easy to overlook, especially if you assume that tired legs or swelling are just part of everyday life. But delaying care increases your risk of serious complications.
Contact a healthcare provider if you notice leg swelling, heaviness, skin discoloration, or visible varicose veins. These can be signs of untreated VRD. If sores appear near the ankles or leg pain disrupts your daily activities, don’t wait. Seek care right away.
Many people also explore holistic vein care to support their well-being. Services like massage, nutrition planning, and stress-reducing therapies can improve circulation and comfort. And if you have risk factors, even without symptoms, preventive care can help protect your vein health over time.
How Vein Health Supports Cardiovascular Wellness
Your veins play a critical role in overall circulation. When blood doesn’t return efficiently to the heart, it puts extra strain on your cardiovascular system. Supporting healthy veins helps maintain steady blood flow and reduces the risk of complications that affect your heart and lungs.
That’s why many people approach vein care as part of a larger wellness plan—combining traditional treatment with lifestyle support through holistic services that address the full picture.
Venous Reflux Disease FAQs
Can venous reflux disease be cured?
VRD isn’t curable, but it’s highly manageable. Many people see lasting relief with treatment and lifestyle changes.
How long does treatment take?
Improvement depends on severity. Some feel better in weeks with compression therapy and lifestyle changes. Minimally invasive procedures can also offer quick relief.
Is venous reflux disease dangerous?
Not life-threatening on its own, but it can lead to skin damage, ulcers, and infection if untreated.
What lifestyle changes help with VRD?
Exercise, healthy eating, weight control, leg elevation, and avoiding long periods of inactivity all help. Supportive care such as massage or nutrition counseling can also make a difference.
Why choose holistic care?
Holistic care near me addresses your full health picture, physical, emotional, and lifestyle, while complementing medical treatment.
Take Control of Your Vein Health
Venous reflux disease is common, but manageable. Early recognition and lifestyle changes can prevent complications and reduce symptoms. With the right combination of care, including medical treatment and wellness support, you can improve your vein health and feel better every day.
Whether you’re managing symptoms or taking preventive steps, don’t wait. Talk to your healthcare provider and explore local resources that support your long-term well-being.
Resources:
https://my.clevelandclinic.org/health/diseases/16872-chronic-venous-insufficiency-cvi