There are many types of vein conditions that people develop over the course of their lifetimes. Many people are genetically predisposed to develop venous issues and suffer with longstanding vein disease, where others breeze through life with just minor vein issues in later years. Anyone who has had vein disease for many years is at increased risk for developing Chronic Venous Insufficiency (often abbreviated as “CVI”). CVI is an umbrella term for the more advanced stages of venous disease. This would include swelling of the ankle and leg, or edema, stasis dermatitis and venous ulcer. Probably the most-common vein condition, and the one most people are familiar with, is the malady of varicose veins. A brief synopsis of each of these vein conditions is discussed below:
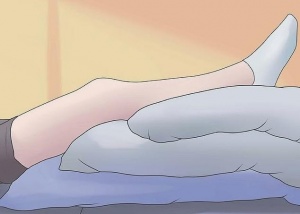
Swelling (a/k/a Edema) – Many patients with CVI suffer from swelling of the ankles and lower legs which begins first thing in the morning and gets progressively worse throughout the day. It results from abnormally elevated pressures in the leg veins. Swelling associated with venous disease may be relieved by periodically elevating the legs throughout the day, or, by donning graduated compression stockings upon arising which will help to diminish the swelling. Treatment may involve Endovenous ablation of the diseased veins.
Stasis Dermatitis – This condition is when leaky valves in leg veins allow the buildup of a higher amount of pressure in those veins. It is also referred to as chronic venous hypertension. It may lead to inflammation of the vein wall and surrounding soft tissues. The increased pressure leads to stasis dermatitis, a darkening, hardening, or thickening of the skin and soft tissues of the lower legs, especially near the ankles. It often ends up as venous ulcers which are difficult to heal. In-office treatments by a vein specialist will bring rapid relief to patients suffering from stasis dermatitis, and the use of compression stockings can help decrease the pressure within the venous system, post-treatment and going forward.
Venous Ulcer – This is the most advanced case of edema and stasis dermatitis and ends as ulcers which form in the damaged tissues. Topical wound care may be attempted, but these ulcers are difficult to heal and may even need the intervention of sessions of antibiotics administered by IV to clear up the ulcer and thwart its return after the IV regimen and/or special wound care is discontinued.
Venous Thrombosis – Venous insufficiency and blood clots (a/k/a venous thrombosis) are closely related. Some people have a genetic predisposition to forming clots, while others suffer a blood clot in a deep vein due to surgery, cancer or trauma from a broken bone. These clots can damage the valves in the veins and lead to chronic venous problems.
Varicose Veins – Common varicose vein symptoms include leg heaviness, leg swelling, throbbing, fatigue, aching, itching, restless legs, and cramps. Most varicose vein problems arise when the valves in leg veins aren’t working to keep the blood moving out of the legs normally. Some of the symptoms associated with varicose veins may be relieved by elevating the legs or wearing compression stockings or resorting to the use of pain medications.
Tips for varicose vein prevention
- Exercise regularly to improve your circulation and improve your overall health. Walking and running are two of the best exercises to help your leg circulation.
- Elevate your legs while you’re resting to let gravity relieve the pressure in your leg veins.
- Avoid putting too much pressure on your legs. Keep your weight under control, avoid repetitive strenuous activities, and don’t keep your legs crossed for prolonged periods of time.
- Be kind to your legs and avoid standing still or sitting for prolonged periods of time. When you are standing, shift your weight from one foot to another, and, when you are sitting, flex your feet up and down or get up and take a walk periodically.
- Wear compression stockings for support in your legs, especially if you will be standing or sitting for a prolonged period of time.
- Eat a healthy diet low in salt and high in fiber because salt contributes to water retention which will cause swelling in the legs, and, fiber helps decrease the risk of constipation which increases pressure on leg veins



