Modern healthcare is in a state of constant evolution. As medical advancements redefine the possibilities of treatment, patient care, and disease management, so too does our understanding of where and how patients should receive care. In recent years, there’s been a palpable shift away from the sterile, impersonal corridors of hospitals for long-term treatment. The emergence of chronic conditions, advancements in home medical equipment, and a deeper appreciation for mental well-being have combined to spotlight a venue we often overlook in the context of healthcare: the patient’s own home.
At the crux of this evolution is the acknowledgment of holistic well-being—where the physical, emotional, and psychological dimensions of health are intertwined. Traditional hospital settings, while indispensable for acute care and surgical procedures, may not always be conducive to this comprehensive approach, especially for prolonged treatments or recovery. The stark lights, unfamiliar sounds, and the inevitable feeling of detachment can sometimes exacerbate stress and delay recovery.
Enter the domain of in-home care, a concept as old as the practice of medicine itself, but one that’s gaining renewed importance. With an aging global population and the rising prevalence of conditions that require long-term care, the home emerges not just as a place of comfort, but a viable, often preferable, venue for medical care. It represents familiarity, solace, and a semblance of normalcy in the face of challenging medical conditions.
In this exploration, we’ll delve into the various facets of home-based care, spotlighting its significance in the landscape of modern medicine and chronic conditions. From the challenges faced in traditional hospital-based care to the advantages of healing in familiar surroundings, we aim to paint a comprehensive picture of why home might indeed be where the heart—and health—is.
The Reality of Chronic Conditions
The term ‘chronic condition’ often evokes a sense of permanence and persistence. In the realm of medical terminology, a chronic condition is defined as a health problem that lasts over a year, requires ongoing medical attention, and may or may not have a resolution. But beyond the clinical definitions, chronic conditions cast long shadows on the lives of patients and their families, encompassing a broad spectrum of ailments, each with its unique challenges and complications.
Consider Alzheimer’s disease, a neurodegenerative disorder characterized by progressive memory loss, impaired reasoning, and personality changes. The World Health Organization estimates that around 50 million people worldwide have dementia, with Alzheimer’s disease accounting for 60-70% of these cases. The insidious nature of Alzheimer’s is not just in its physiological manifestations, but in its emotional impact. As memory fades, so do the shared experiences, moments, and bonds that define relationships. Families watch as their loved ones, though present physically, drift into a realm where recognition and recollection become fleeting.
Similarly, Parkinson’s disease, another neurodegenerative condition, is marked by tremors, rigidity, and bradykinesia (slowness of movement). Beyond the physical, Parkinson’s often brings with it a suite of non-motor symptoms, including sleep disturbances, depression, and cognitive challenges. The journey of a Parkinson’s patient is one of adaptation, as they and their caregivers learn to navigate the shifting sands of capability and independence.
Then there’s the aftermath of a stroke, a sudden interruption in the brain’s blood supply. While the initial event is acute, its repercussions can be long-lasting. Some survivors grapple with paralysis, speech impairments, and memory problems. The road to recovery can be winding, demanding not just physical rehabilitation but also psychological support as patients reconcile with their altered realities.
These are but a few illustrations in the vast tapestry of chronic conditions. Each ailment, be it diabetes, chronic obstructive pulmonary disease (COPD), or arthritis, brings with it not just a set of symptoms, but a lived experience. Patients and their families navigate daily challenges, from medication management to lifestyle adjustments, often seeking a semblance of normalcy amidst the disruptions.
What becomes evident is that the management of chronic conditions is not just about medical interventions but encompasses a broader ecology of care. The physical environment, psychological support, and a structured routine play pivotal roles in determining the quality of life for patients. And this is where the traditional hospital setting sometimes falls short, prompting a shift towards in-home care for chronic conditions.
The Challenges of Hospital-Based Care
Hospitals, often seen as the epicenters of medical intervention and recovery, undoubtedly play a pivotal role in acute healthcare scenarios. From sophisticated surgical procedures to managing emergency cases, hospitals are equipped with the tools, personnel, and protocols to handle immediate and often life-threatening situations. However, when it comes to the long-term management and care of chronic conditions, the hospital environment, despite its merits, can present several challenges.
1. Emotional Strain: Hospital stays, especially extended ones, can take an emotional toll on patients. The sterile environment, away from the comforts and familiarity of home, can exacerbate feelings of isolation. The constant hum of medical machinery, coupled with the periodic flurry of medical staff, can disrupt a patient’s sense of peace and personal space. Such settings can be particularly distressing for patients with cognitive disorders like Alzheimer’s, who rely heavily on familiar surroundings and routines to navigate their day-to-day lives.
2. Financial Impact: Long-term hospital care is expensive. Even with insurance, out-of-pocket expenses can quickly accumulate, placing an immense financial burden on patients and their families. From bed charges to diagnostic tests, medications, and specialist consultations, the costs pile up, often overshadowing the primary concern of healthcare with financial anxieties.
3. Risk of Hospital-Acquired Infections: Though hospitals maintain stringent cleanliness standards, the risk of acquiring infections – often resistant to multiple antibiotics – remains a genuine concern. Prolonged hospital stays can expose patients to pathogens, potentially leading to complications that can further extend their stay or, worse, lead to life-threatening conditions.
4. Limited Personalized Attention: Due to the sheer volume of patients, hospitals often operate on structured routines. While this is essential for organizational efficiency, it may not always align with an individual patient’s needs. The ratio of nursing staff to patients can also mean that personalized, continuous attention is not always feasible, especially during peak times or emergencies.
5. Diminished Autonomy: Hospital routines can sometimes feel rigid to patients used to their own daily rhythms. Fixed meal times, regimented medication schedules, and restrictions on movement or activities can make patients feel a loss of control over their lives. This diminished autonomy can impact their overall well-being and mental health, especially if they feel they’re just another patient rather than an individual with unique needs and preferences.
6. Family Inconvenience: While family members and close friends are eager to support their loved ones during hospital stays, frequent visits can disrupt their routines. Balancing work, home responsibilities, and hospital visits can be draining. Additionally, hospital visiting hours might not always align with their availability, limiting the support a patient receives.
In summary, while hospitals provide critical services and are indispensable in acute medical situations, they are not always the most conducive environments for the long-term care and recovery of patients with chronic conditions. As the medical community recognizes these challenges, there’s been a growing emphasis on alternative care environments that offer both medical attention and emotional support. The surge in home-based care solutions stems from this understanding, aiming to blend medical rigor with the warmth and familiarity of home.
The Shift to Home-Based Care
The evolution of the healthcare landscape in recent years has borne witness to a notable shift from traditional hospital-based care to more patient-centric home-based care models. Several factors have fueled this transition, underscoring the need to prioritize patient well-being, convenience, and cost-effectiveness. Here’s a deep dive into why home-based care is emerging as a viable and often preferable alternative for many.
1. Comfort and Familiarity: At the core of home-based care is the undeniable comfort of one’s own home. Patients recover in familiar surroundings, surrounded by their personal belongings, cherished memories, and loved ones. This familiar environment often accelerates the healing process, reduces stress, and boosts the overall morale of the patient.
2. Personalized Care: In-home care offers a tailored approach to patient care. Caregivers can provide one-on-one attention, ensuring that the specific needs and preferences of the patient are addressed. This individualized attention often translates to more comprehensive and nuanced care, from customized meal plans to personalized therapy sessions.
3. Reducing Rehospitalizations: A significant advantage of home-based care is the reduced risk of readmissions. By receiving personalized care and close monitoring in a home setting, potential issues can be identified and addressed promptly, often preventing the need for rehospitalization.
4. Cost-Effectiveness: On a comparative scale, home-based care can be more affordable than prolonged hospital stays. Without the overhead costs associated with institutional care, patients and their families can often achieve significant savings, all while receiving top-notch care.
5. Flexibility for Families: Home-based care offers flexibility not just for the patient but also for their families. Loved ones can be more involved in the patient’s care, understanding their needs, and collaborating with caregivers to create the best care plan. The elimination of travel time to and from the hospital also eases logistical burdens.
6. Integration of Technology: The rise of telemedicine and advanced health monitoring gadgets has made in-home care more efficient than ever. Patients can now be monitored remotely, with data being sent directly to healthcare professionals. This seamless integration of technology ensures that patients receive timely interventions, even from the comfort of their homes.
7. Emphasis on Holistic Well-being: Beyond just medical care, home-based care often places a strong emphasis on the holistic well-being of the patient. This includes physical therapy, occupational therapy, psychological counseling, and even recreational activities tailored to the patient’s interests and capabilities.
8. Empowerment and Autonomy: One of the unsung benefits of home care is the sense of autonomy it restores to patients. They have a say in their daily routines, their meals, and even the pace at which they wish to undergo therapies. This empowerment plays a crucial role in improving their self-worth and overall mental health.
In light of these benefits, it’s evident that home-based care is not just an alternative but often a preferred choice for many. As healthcare continues to evolve, the emphasis on patient well-being, both physical and emotional, drives the need for solutions that are both medically sound and emotionally nurturing. Home-based care, with its myriad advantages, stands out as a beacon in this new era of healthcare.
Empowering Modern Healthcare with Comprehensive Home Care Solutions
In the constantly evolving panorama of healthcare, the emergence and growth of home-based care signal a revolutionary shift. As we’ve delved into the complexities of hospital-based care and the inherent challenges it presents, the alternative of home care shines with promise. This isn’t just about medicine or therapy; it’s about nurturing the human spirit, allowing patients to recover in the warmth of their homes, and ensuring their journey to wellness is as comfortable and effective as possible.
The transition from hospital wards to living room couches isn’t merely logistical; it’s deeply emotional. With chronic conditions on the rise and the increasing awareness of their multifaceted challenges, the healthcare industry had to innovate. Home care, with institutions like HWCG leading the charge, meets these challenges head-on. Tailored care plans, advanced technology integrations, and the undeniable advantage of familiar surroundings make in-home care a robust and compassionate solution.
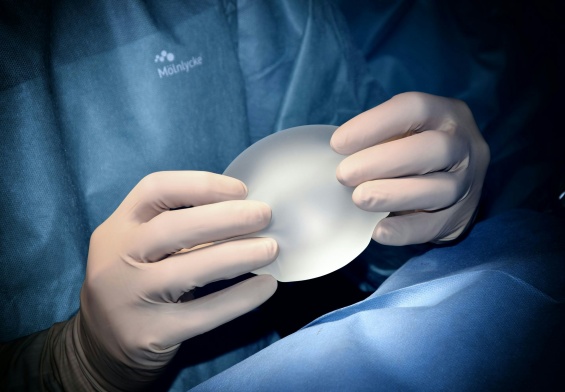
Furthermore, the symbiosis between surgical advancements, such as those offered by renowned practitioners in fields like plastic surgery, and the post-operative care provided by home caregivers, exemplifies the future of healthcare. This cohesive approach ensures that patients not only undergo life-altering procedures but also have the support they need afterward.
As we look forward, the narrative is clear: modern healthcare isn’t just about treating illnesses; it’s about enhancing the quality of life. Home-based elder care, with its profound advantages and patient-first approach, is pivotal in crafting this new narrative, proving that the best place for recovery and long-term care can often be where the heart is – at home.