Back pain is one of the most common complaints among adults over the age of 65. For many seniors, it can go beyond a minor annoyance—chronic pain in the back can lead to limited mobility, disrupted sleep, and even depression due to decreased independence.
Understanding the causes of back pain in seniors is the first step toward finding relief and improving quality of life. In many cases, a tailored home care plan can help manage symptoms, prevent injuries, and support seniors in maintaining their daily routines safely and comfortably.
Why Is Back Pain So Common in Older Adults?
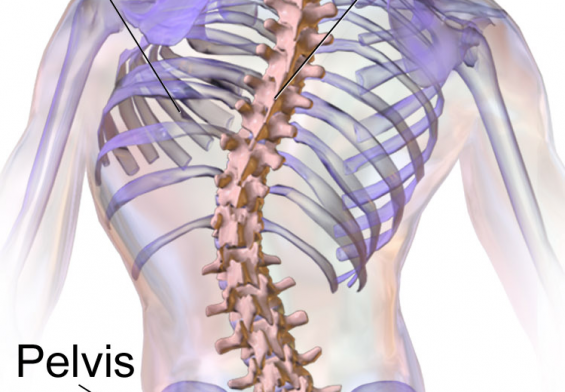
As we age, the structures that support our spine—bones, muscles, discs, and joints—naturally begin to weaken. Years of strain, injury, or poor posture catch up over time, and even everyday activities like bending over, standing up, or climbing stairs can become painful.
Let’s explore the most frequent causes of back pain among seniors.
1. Degenerative Disc Disease
The spine is made up of vertebrae cushioned by discs that act like shock absorbers. Over time, these discs can dry out, shrink, or become damaged. This age-related condition is known as degenerative disc disease.
Symptoms include:
-
Persistent lower back pain
-
Pain that worsens with bending or twisting
-
Stiffness in the morning or after sitting
While this condition is common, it can severely impact mobility, especially without physical activity or proper support.
2. Osteoarthritis of the Spine
Osteoarthritis affects the joints and is particularly common in the spine among seniors. The cartilage that cushions joints wears down, causing bones to rub against each other. This leads to:
-
Inflammation
-
Stiffness
-
Localized back pain
In advanced cases, bone spurs can form and press against nearby nerves, amplifying the discomfort.
3. Spinal Stenosis
Spinal stenosis occurs when the spinal canal narrows and compresses the nerves. It’s a frequent cause of back and leg pain in older adults and often makes walking difficult.
Symptoms include:
-
Pain or numbness when standing or walking
-
Relief when leaning forward or sitting
-
Weakness in legs or feet
This condition can affect seniors’ ability to move around safely, making them more prone to falls or dependency on others.
4. Osteoporosis and Compression Fractures
Osteoporosis causes bones to lose density and strength. In seniors, this can result in compression fractures in the vertebrae, leading to:
-
Sudden, severe back pain
-
Loss of height
-
A stooped posture
These fractures often go undiagnosed, as they may be mistaken for general back pain or aging symptoms.
5. Lifestyle and Posture Issues
Not all back pain stems from disease. Common lifestyle factors in seniors can contribute to chronic pain as well, such as:
-
Poor posture, especially when sitting or walking
-
Lack of core muscle strength due to inactivity
-
Improper lifting techniques when handling even light objects
Over time, these habits can strain muscles and joints, leading to discomfort and loss of mobility.
6. Underlying Medical Conditions
Several health conditions can manifest as back pain, including:
Sciatica
Pain radiating from the lower back into the leg due to sciatic nerve compression.
Fibromyalgia
A condition characterized by widespread musculoskeletal pain, fatigue, and tenderness.
Kidney Issues
Infections or stones can cause pain that mimics lower back discomfort but may require urgent treatment.
Proper diagnosis is key—something caregivers can help monitor and communicate to healthcare providers if symptoms worsen.
When Back Pain Begins to Interfere With Daily Life
Back pain isn’t just a physical issue—it can affect every part of a senior’s life:
-
Struggling to walk, climb stairs, or get out of bed
-
Needing help with hygiene due to pain or stiffness
-
Avoiding social outings due to mobility concerns
-
Relying on painkillers can lead to other complications
Chronic pain can also lead to sleep disturbances, depression, and feelings of isolation. That’s where home care services can provide meaningful, compassionate support.
How Home Care Services Can Help Seniors With Back Pain
Home care isn’t just for people with major illnesses—it’s also valuable for those dealing with everyday challenges like back pain.
Here’s how professional caregivers can help:
-
Mobility Assistance: Helping seniors move around safely, reducing fall risk
-
Personal Care Support: Bathing, dressing, and grooming without strain
-
Pain Management Reminders: Ensuring medications are taken properly and on time
-
Transportation to Appointments: So, back pain doesn’t delay essential medical care
-
Physical Activity Encouragement: Gentle stretches or prescribed exercises, guided with care
-
Home Safety Improvements: Recommending tools like grab bars, supportive chairs, or fall-proof layouts
Even a few hours of weekly care can dramatically improve comfort, independence, and safety for seniors living with chronic back pain.
Tips to Help Prevent and Manage Back Pain in Seniors
While not all back pain is preventable, many cases can be managed through healthy habits and proper support:
-
Stretch Regularly: Gentle yoga or guided exercises to maintain flexibility
-
Use Ergonomic Seating: Supportive chairs and cushions protect the spine
-
Monitor Bone Health: Get regular bone density scans and ensure enough calcium and vitamin D
-
Make the Home Senior-Friendly: Avoid slippery floors, install support rails, and remove trip hazards
Home care professionals often work with families to implement these changes and help seniors stay comfortable at home longer.
Conclusion: Aging With Comfort Is Possible
Back pain in seniors is common, but it doesn’t have to lead to a decline in quality of life. From degenerative disc disease to lifestyle strain, understanding the root causes helps families act early and explore appropriate care.
Whether your loved one needs help getting dressed, preparing meals, or simply staying mobile, home care services can fill in the gaps, making daily life more manageable and less painful.
-
National Institute on Aging – Back Pain
https://www.nia.nih.gov/health/back-pain -
Mayo Clinic – Back Pain
https://www.mayoclinic.org/diseases-conditions/back-pain/symptoms-causes