Chronic Heart Disease: A Closer Look
Heart disease is a broad term that covers various conditions affecting the heart and blood vessels. It remains a leading cause of death globally, impacting millions of lives each year. Let’s explore the different types of heart disease and what they entail.
Types of Heart Disease: A Deeper Dive
Coronary Artery Disease (CAD)
Coronary Artery Disease is the most common type of heart disease. It happens when the arteries that supply blood to the heart become narrowed due to a buildup of plaque. This plaque is made up of cholesterol, fatty substances, cellular waste products, calcium, and fibrin, which restricts blood flow to the heart.
- Stable Angina: Chest pain or discomfort that occurs predictably with exertion and is relieved by rest or medication.
- Unstable Angina: Chest pain that occurs at rest or with minimal exertion, indicating a more severe blockage.
- Heart Attack: Occurs when blood flow to a part of the heart is abruptly blocked, causing heart muscle damage.
Heart Failure
Heart failure, also known as congestive heart failure, occurs when the heart muscle weakens and can’t pump enough blood to meet the body’s needs.
- Systolic Heart Failure: The heart can’t pump blood effectively out of the heart.
- Diastolic Heart Failure: The heart can’t properly fill with blood.
Arrhythmias
Arrhythmias are irregular heartbeats that can disrupt normal heart function.
- Bradycardia: A slow heart rate.
- Tachycardia: A rapid heart rate.
- Atrial Fibrillation: A common type of irregular heartbeat that can increase stroke risk.
- Ventricular Fibrillation: A life-threatening arrhythmia where the heart’s lower chambers quiver ineffectively.
Cardiomyopathy
Cardiomyopathy is a disease of the heart muscle that makes it harder for the heart to pump blood.
- Dilated Cardiomyopathy: The heart’s main pumping chamber (left ventricle) becomes enlarged and weakened.
- Hypertrophic Cardiomyopathy: The heart muscle becomes abnormally thick, making it harder for the heart to pump blood.
- Restrictive Cardiomyopathy: The heart muscle becomes stiff, making it difficult for the heart to fill with blood.
Congenital Heart Defects
Congenital heart defects are structural abnormalities of the heart present at birth. They can range from mild to severe and may require lifelong care.
Valvular Heart Disease
Valvular heart disease occurs when one or more of the heart’s four valves doesn’t function properly.
- Stenosis: The valve opening is narrowed, restricting blood flow.
- Regurgitation: The valve doesn’t close tightly, allowing blood to leak backward.
Risk Factors for Heart Disease: A Closer Look
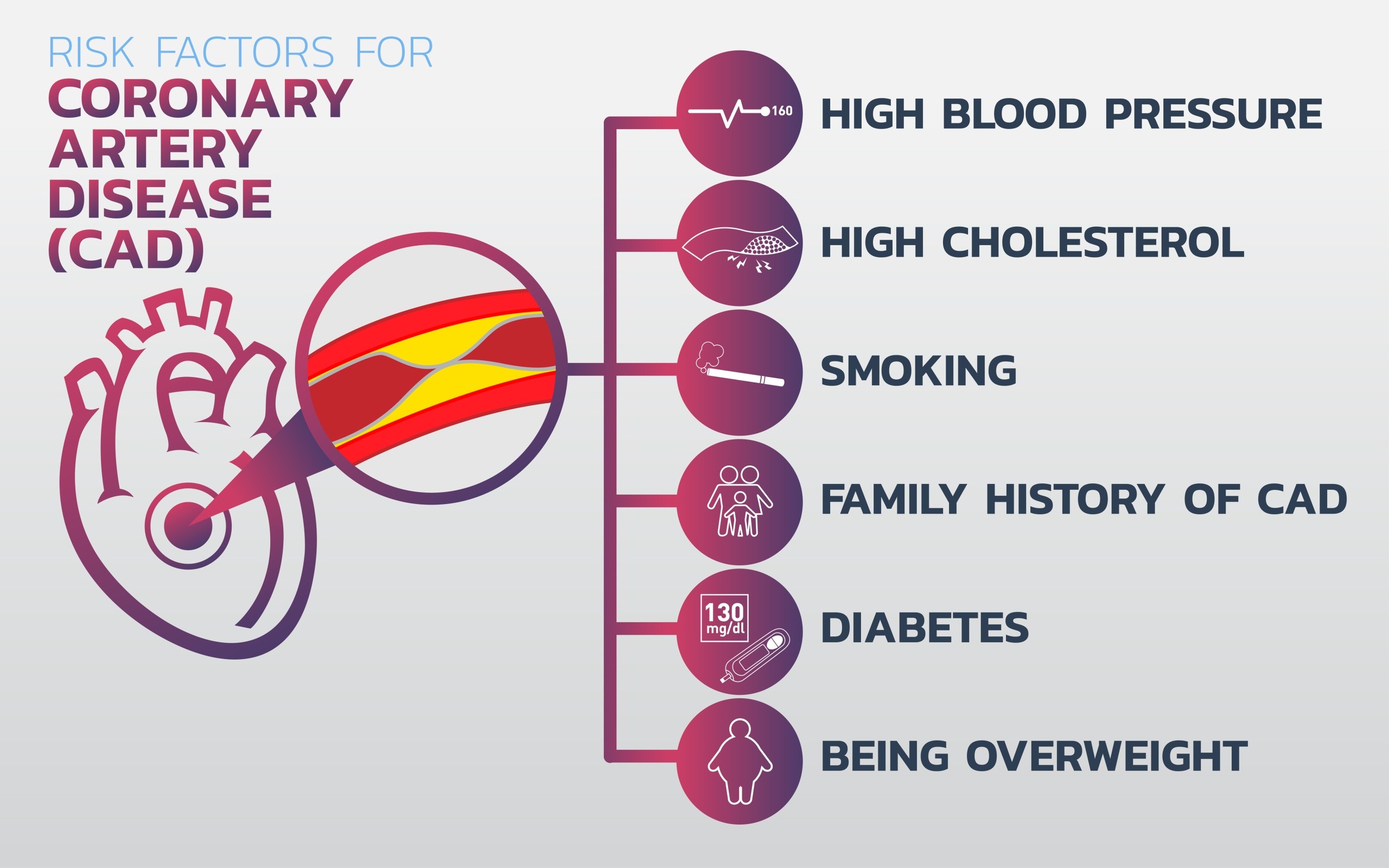
Understanding the risk factors for heart disease is essential for prevention and management. Let’s dig deeper into each factor and see how they contribute to the development of heart disease.
High Blood Pressure (Hypertension)
High blood pressure, or hypertension, forces the heart to work harder than normal to pump blood throughout the body. Over time, this increased workload can lead to the thickening of the heart muscle, which can cause the heart to function less efficiently.
- Impact: Can damage arteries, making them less elastic, which decreases the flow of blood and oxygen to the heart.
- Management: Regular monitoring, medication, reduced salt intake, and lifestyle changes like exercise can help manage hypertension.
High Cholesterol
Cholesterol is a fatty substance that’s necessary for building cells, but too much of it can be harmful. High levels of low-density lipoprotein (LDL) cholesterol can lead to plaque buildup in arteries, restricting blood flow to the heart.
- Impact: Can lead to the formation of plaque in the arteries, increasing the risk of coronary artery disease and heart attacks.
- Management: Diet, exercise, and medications can help control cholesterol levels.
Smoking
Smoking damages the lining of the arteries, leading to a buildup of fatty material (atheroma) which narrows the artery. This can cause angina, heart attack, or stroke.
- Impact: Increases blood pressure, reduces oxygen to the heart, and raises heart rate. Also contributes to clot formation.
- Management: Quitting smoking can significantly reduce the risk of heart disease. Support groups, nicotine replacement therapy, and medications can aid in quitting.
Diabetes
Diabetes increases the risk of heart disease due to high blood sugar levels, which can damage blood vessels and the nerves that control the heart.
- Impact: High glucose levels can lead to increased plaque formation and inflammation in the blood vessels.
- Management: Controlling blood sugar through diet, exercise, medication, and regular monitoring can reduce the risk.
Obesity
Obesity is linked to various risk factors such as high blood pressure, high cholesterol, and diabetes. Excess weight can strain the heart and contribute to the development of heart disease.
- Impact: Increases the likelihood of high blood pressure, high cholesterol, and diabetes, all of which are risk factors for heart disease.
- Management: Weight loss through a balanced diet, regular physical activity, and behavioral changes can significantly reduce the risk.
Physical Inactivity
A sedentary lifestyle is a major risk factor for heart disease. Lack of exercise contributes to obesity, high blood pressure, high cholesterol, and diabetes.
- Impact: Increases the risk of developing other heart disease risk factors.
- Management: Engaging in regular physical activity, such as walking, running, swimming, or cycling, can improve heart health.
Unhealthy Diet
A diet high in saturated fats, trans fats, salt, and sugar can contribute to the development of heart disease. Poor nutrition can lead to high cholesterol, high blood pressure, and obesity.
- Impact: Increases risk of plaque buildup in arteries, leading to coronary artery disease and heart attacks.
- Management: Eating a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help maintain heart health.
Excessive Alcohol Consumption
Excessive drinking can raise blood pressure, contribute to high cholesterol, and increase the risk of heart disease.
- Impact: Can lead to high blood pressure, heart failure, and even stroke.
- Management: Moderation is key. Limiting alcohol intake to recommended levels can reduce the risk.
Family History
A family history of heart disease can increase your risk, indicating a genetic predisposition. While you can’t change your family history, being aware of it can help you take preventive measures.
- Impact: Genetic factors can contribute to high blood pressure, high cholesterol, and other heart disease risk factors.
- Management: Regular check-ups and early intervention, along with a heart-healthy lifestyle, can help manage the risk.
By understanding and addressing these risk factors, you can take proactive steps to protect your heart and overall health. Regular medical check-ups, a healthy lifestyle, and awareness of your personal risk factors are key to preventing heart disease.
Symptoms of Heart Disease: A Closer Look
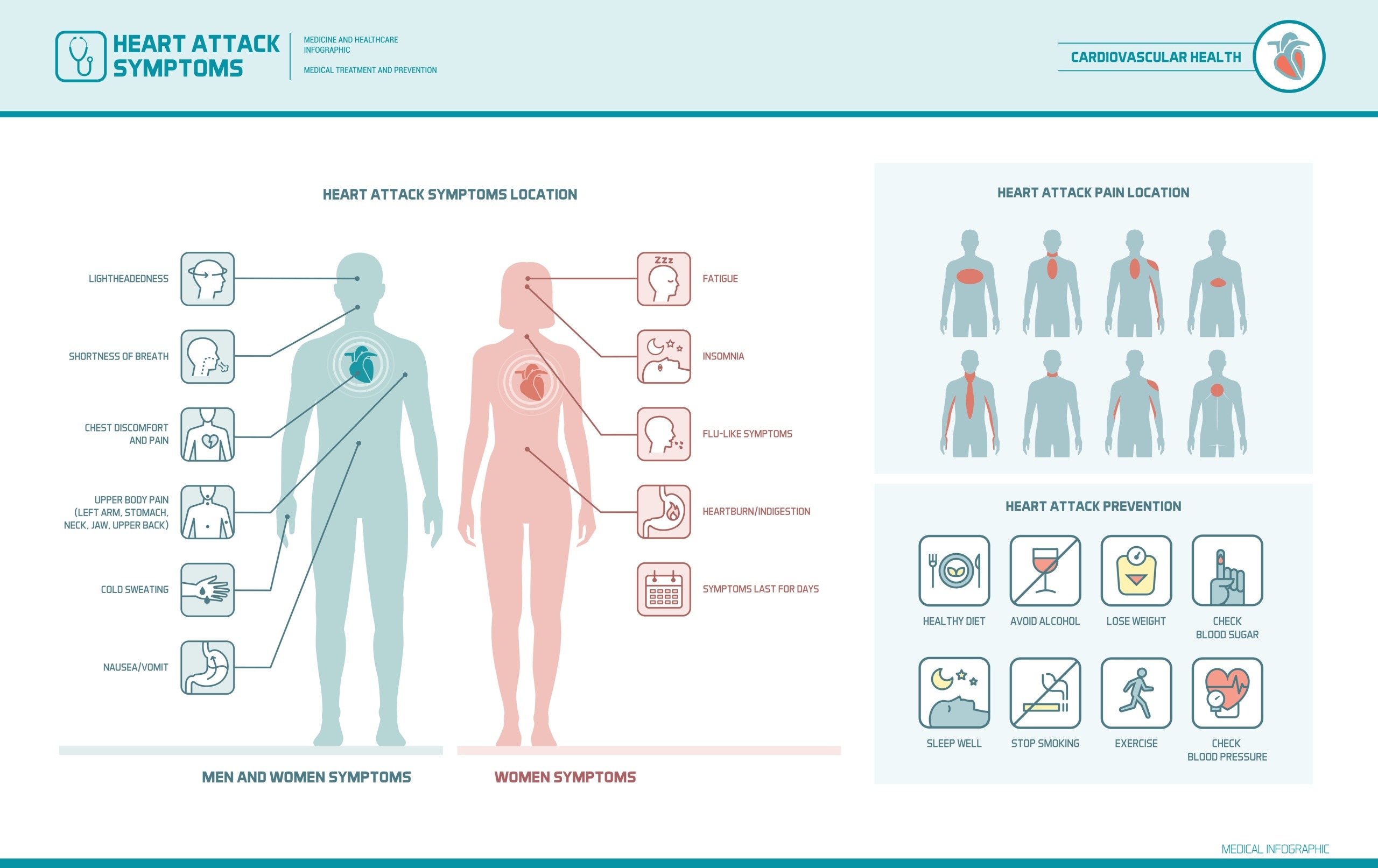
Heart disease can manifest in various ways, and the symptoms can vary depending on the specific type of heart condition. Recognizing these symptoms early can lead to timely medical intervention and better management of the disease.
Chest Pain or Discomfort
Often referred to as angina, chest pain is a common symptom of heart disease. It can feel like pressure, squeezing, fullness, or pain in the center of the chest.
- Angina: May occur during physical activity or stress and typically goes away with rest.
- Heart Attack: Intense and persistent chest pain that may spread to the arms, back, neck, jaw, or stomach.
Shortness of Breath
Difficulty breathing can occur with minimal exertion or even at rest. It is often a sign that the heart isn’t pumping effectively.
- Heart Failure: The heart’s inability to pump enough blood can cause fluid buildup in the lungs, leading to shortness of breath.
- Heart Attack: Shortness of breath can also be a warning sign of a heart attack.
Fatigue
Unusual fatigue or extreme tiredness can be a symptom of heart disease, especially in women. It may be due to the heart’s decreased ability to pump blood efficiently.
- Heart Failure: Reduced blood flow can cause persistent fatigue and weakness.
- Coronary Artery Disease: Limited blood flow to the heart muscle can lead to feelings of exhaustion.
Swelling in the Ankles or Feet
Edema, or swelling in the ankles, feet, or legs, can indicate heart disease. It results from the heart’s inability to pump blood effectively, leading to fluid buildup in the body.
- Heart Failure: Fluid retention is a common symptom of heart failure.
- Valvular Heart Disease: Improper functioning of the heart valves can also lead to fluid accumulation.
Irregular Heartbeat
Arrhythmias, or irregular heartbeats, can cause the heart to beat too fast, too slow, or irregularly. They may feel like fluttering, pounding, or racing in the chest.
- Atrial Fibrillation: A common type of arrhythmia that increases the risk of stroke.
- Ventricular Fibrillation: A life-threatening condition where the heart’s lower chambers quiver ineffectively.
Dizziness or Lightheadedness
Feeling dizzy or lightheaded can be a sign of a heart problem. It may occur due to a drop in blood pressure or an arrhythmia affecting blood flow to the brain.
- Heart Failure: Poor blood circulation can lead to dizziness.
- Arrhythmias: Irregular heartbeats can disrupt blood flow, causing lightheadedness.
Prevention and Management of Heart Disease: A Closer Look
Adopting a heart-healthy lifestyle is essential for both preventing and managing heart disease. Here are some detailed strategies to help protect your heart.
Healthy Eating
A balanced diet can significantly reduce the risk of heart disease. Focus on foods that support heart health and avoid those that can harm it.
- What to Eat: Fruits, vegetables, whole grains, lean proteins, and healthy fats (like those found in fish, nuts, and olive oil).
- What to Avoid: Saturated fats, trans fats, excess salt, and added sugars.
Regular Exercise
Physical activity strengthens the heart and improves overall cardiovascular health. Aim for at least 150 minutes of moderate-intensity exercise each week.
- Types of Exercise: Brisk walking, cycling, swimming, and other aerobic activities.
- Benefits: Helps control weight, reduces blood pressure, improves cholesterol levels, and boosts overall heart health.
Weight Management
Maintaining a healthy weight is crucial for reducing the risk of heart disease. Obesity is linked to several risk factors, including high blood pressure, high cholesterol, and diabetes.
- Strategies: Combine a healthy diet with regular physical activity.
- Goals: Aim for a body mass index (BMI) within the normal range (18.5-24.9).
Smoking Cessation
Quitting smoking is one of the best things you can do for your heart. Smoking damages blood vessels and increases the risk of heart disease.
- Support: Seek help from support groups, nicotine replacement therapy, and medications.
- Benefits: Reduces the risk of coronary artery disease, heart attacks, and other cardiovascular problems.
Stress Management
Chronic stress can contribute to heart disease by increasing blood pressure and promoting unhealthy behaviors (such as overeating or smoking).
- Techniques: Practice relaxation techniques like deep breathing, meditation, yoga, or mindfulness.
- Activities: Engage in hobbies, spend time with loved ones, and ensure adequate rest and sleep.
Regular Health Check-ups
Regular medical check-ups are essential for monitoring heart health and detecting any potential issues early.
- Screenings: Blood pressure, cholesterol levels, blood sugar levels, and weight.
- Follow-ups: Regular visits with your healthcare provider to manage existing conditions and adjust treatment plans as needed.
The Role of In-Home Care in Managing Heart Disease
For individuals living with heart disease, in-home care can provide essential support and improve quality of life. Here’s how in-home care can make a significant difference:
- Personalized Care at Home
- In-home care services offer personalized care plans tailored to the individual needs of those with heart disease. This ensures that patients receive the right support and monitoring to manage their condition effectively.
- Continuous Monitoring
- In-home caregivers can assist with continuous monitoring of heart health indicators like blood pressure and cholesterol levels. Regular monitoring helps detect any changes or complications early, allowing for timely intervention.
- Medication Management
- Managing medications can be challenging, especially for those with complex heart disease treatment regimens. In-home caregivers help ensure patients take their prescribed medicines correctly and on time, reducing the risk of missed doses or incorrect usage.
- Lifestyle Support
- In-home care can support a heart-healthy lifestyle by assisting with meal planning and preparation, encouraging physical activity, and providing companionship to reduce stress. Caregivers can help patients adhere to dietary recommendations and stay active, which is crucial for managing heart disease.
- Emergency Response
- Having trained in-home care professionals can be lifesaving. Caregivers are trained to recognize the signs of heart-related emergencies and take immediate action, ensuring patients receive prompt medical attention.
- Family Support
- In-home care services provide peace of mind and support for family members, knowing their loved one is being cared for by professionals. This allows family members to focus on their own well-being and spend quality time with their loved ones without the added stress of caregiving duties.
Conclusion: Taking Control of Heart Health
Understanding the different types of heart disease, recognizing the symptoms, and knowing the risk factors are essential steps in taking control of your heart health. Adopting a heart-healthy lifestyle, managing risk factors, and seeking regular medical care can help prevent and manage heart disease effectively.
For those living with heart disease, in-home care services offer invaluable support, ensuring personalized care, continuous monitoring, and a better quality of life. If you or a loved one is dealing with heart disease, consider the benefits of in-home care as part of your comprehensive management plan.
By staying informed and proactive, you can protect your heart and enjoy a healthier, more fulfilling life.