Hearing “you might need back surgery” can feel like a worst-case scenario—but it’s a lot more common than you think. In the U.S. alone, more than 300,000 lumbar spinal fusions are performed every year, and low back pain affects hundreds of millions of people worldwide, making it one of the leading causes of disability.
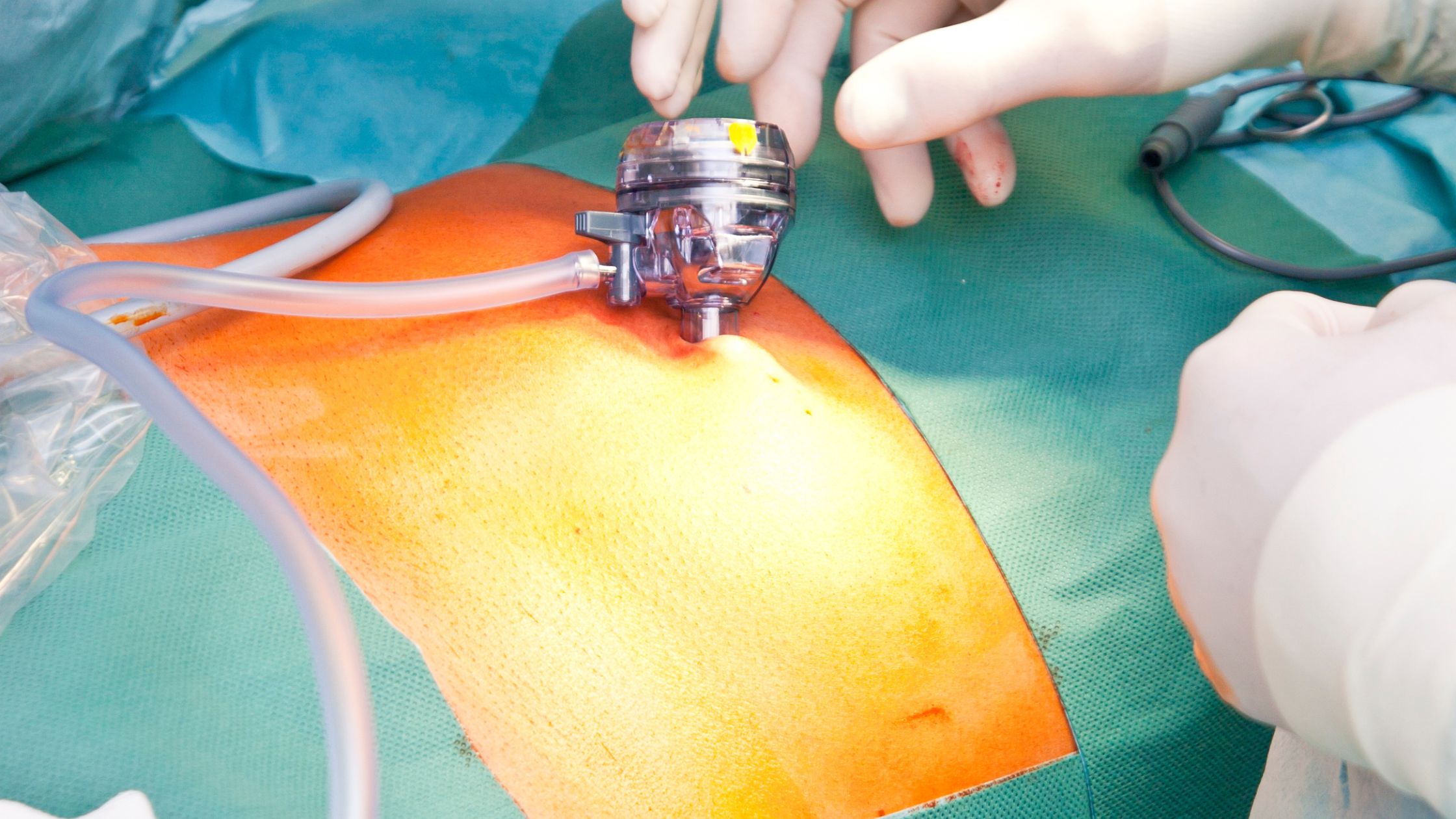
Here’s the twist: while “back surgery” still sounds scary, many modern procedures are now done using minimally invasive spine surgery—small incisions, less muscle damage, and a faster recovery compared to traditional open surgery. Patients often go home sooner and get back to daily life faster, instead of facing weeks in a hospital bed the way older stories suggest.
You don’t have to pretend you’re not afraid. But understanding how minimally invasive techniques actually work can turn that fear into a clear, realistic plan for getting your life back.
Quick Answer: What Makes Minimally Invasive Spine Surgery Less Scary?
Minimally invasive spine surgery uses small incisions and special tools (often with a camera) to treat spine problems while disturbing less muscle and tissue.
For many patients, that can mean:
- Smaller scars
- Less blood loss
- Less postoperative pain
- Shorter hospital stays
- A faster return to work and normal life
Why Back Surgery Has Such a Scary Reputation
Most of the fear around back surgery comes from old stories:
- Relatives who were in the hospital for a week or more
- Large incisions across the back or neck
- Long periods in bed
- Uncertainty about whether surgery would even “work”
Those experiences were real for people who had back surgery many years ago. But the tools, techniques, and safety standards in spine care have advanced a lot.
Today, surgeons are often able to treat many common problems — like herniated discs or spinal stenosis — through much smaller incisions and more precise approaches.
The goal is the same: take pressure off the nerves and stabilize the spine when needed. The difference is how that goal is reached.
Open vs Minimally Invasive Spine Surgery: What’s the Difference?
Here’s a simple comparison you can use to help readers understand the basics:
| Feature | Traditional “Open” back Surgery | Minimally Invasive Surgery |
| Incision Size | Larger incision, more tissue exposed | Smaller incisions, often less than a few centimeters |
| Muscle Disruption | Muscles are pulled aside more widely | Muscles are spread through small tubes or dilators |
| Blood Loss | Usually greater | Often less |
| Hospital Stay | Longer stay is more common | Many patients go home sooner, sometimes same day |
| Postoperative Pain | Can be more intense at first | Often less, due to less tissue trauma |
| Recovery Time | May be longer | Many patients resume light activity sooner |
Not every patient or condition is a match for minimally invasive techniques, and not every minimally invasive surgery is “easy.” But this kind of table helps take the mystery out of what the term really means.
What Actually Happens Before Minimally Invasive Spine Surgery
Fear thrives in the unknown. Once you understand the process, things often feel more manageable.
1. Evaluation and diagnosis
Before surgery is even on the table, a spine specialist will:
- Take a detailed history of your pain and symptoms
- Perform a physical and neurologic exam
- Review imaging such as X-rays, MRI, or CT scans
You and your surgeon will talk about what is causing your pain and which options you have, including non-surgical treatments, which are often tried first when safe.
2. Deciding if minimally invasive surgery is right for you
Your surgeon will consider:
- The type and location of the problem (like a disc herniation or spinal stenosis)
- Your overall health and any medical conditions
- Your goals — pain relief, walking farther, returning to work, etc.
Not every operation can be done with a minimally invasive approach, but many routine spine procedures can.
3. Pre-surgery planning
You’ll usually:
- Review medications (some may need to be stopped before surgery)
- Get basic lab tests and clearance if needed
- Receive instructions about eating, drinking, and arrival time
What to Expect on the Day of Minimally Invasive Spine Surgery
While every hospital and surgeon is a little different, many patients go through a day that looks something like this:
Before surgery
- You arrive at the surgery center or hospital and check in.
- A nurse reviews your information and starts an IV.
- You meet with your anesthesiologist and surgeon, who answer last-minute questions.
During surgery
- You receive anesthesia so you’re asleep and comfortable.
- The surgeon makes one or a few small incisions, using special instruments and often a camera system or microscope.
- The problem area — like a disc pressing on a nerve — is carefully treated while sparing as much healthy tissue and muscle as possible.
The specifics depend on the type of surgery (for example, a decompression vs a fusion), but the idea is the same: treat the cause of your pain in the least disruptive way possible.
After surgery
- You wake up in a recovery area, where your pain and vital signs are monitored.
- Nurses help you sit up, stand, or walk sooner than you might expect, if it’s safe to do so.
- Many minimally invasive procedures allow patients to go home the same day or after a short stay.
Your surgeon’s team will give you clear instructions about activity, wound care, and follow-up.
To read more about MISS, click here
Recovery: How Minimally Invasive Techniques Can Help You Bounce Back Faster
This is where many patients feel the biggest difference compared to what they feared: recovery is often smoother than the stories they’ve heard.
Less disruption, often less pain
Because minimally invasive surgery usually disturbs less muscle and soft tissue, many patients:
- Need less pain medication
- Move more easily in the first days after surgery
- Feel more confident walking, sitting, and standing sooner
You will still have some soreness or discomfort — it’s still surgery — but the intensity and duration may be less than with older open techniques.
Getting back to daily life
Your surgeon will give specific guidelines, but many patients can:
- Return to light activities like short walks within days
- Resume desk work or remote work in a few weeks, depending on the job
- Gradually add more movement, stretching, and strengthening exercises
Everyone heals at a different pace, but the focus is usually on safe, steady progress — not rushed timelines.
Returning to work and exercise
A key fear for many people is, “Will I ever get back to my normal routine?” With the right surgery, good rehab, and healthy habits, many patients do return to:
- Work (often with a gradual ramp-up)
- Gentle exercise like walking, swimming, or low-impact cardio
- Hobbies and family activities they had put on hold
Your long-term outcome depends on many factors — the condition of your spine, your overall health, and how closely you follow recovery instructions — but minimally invasive techniques are designed to support a faster and more active recovery, not block it.
How to Feel More in Control of the Decision
Even with all the facts, surgery is still a big step. Here are a few ways to feel more confident:
- Ask every question you have. A good spine surgeon welcomes questions and explains things in plain language.
- Understand the goal. Is the surgery meant to reduce leg pain, improve walking, stabilize the spine, or all of the above?
- Ask about alternatives. Make sure you know what happens if you choose not to have surgery yet.
- Clarify the recovery plan. Ask what the first week, first month, and first three months might look like.
You’re not just a spine on a scan. You’re a person with work, family, and a life to get back to. Your care plan should reflect that.
Key Takeaways
- Fear of back surgery is normal, but many stories are based on older, more invasive procedures.
- Minimally invasive spine surgery uses smaller incisions and special tools to reduce muscle and tissue damage.
- This often leads to less pain, shorter hospital stays, and a quicker return to daily life compared with traditional open surgery.
- A detailed guide like “Minimally Invasive Spine Surgery: What to Expect Before, During & After” can help patients understand each step of the process.
- Resources such as “Life After Spine Surgery: Tips for Returning to Work, Exercise & Normal Life” can support recovery planning and set realistic expectations.
- You don’t have to decide on surgery today, but getting clear information now can turn a scary diagnosis into a structured, hopeful plan.
With the right surgeon, the right technique, and a clear recovery roadmap, back surgery doesn’t have to be a horror story. For many people, it becomes the turning point where life starts opening back up again.
Reference Links
- WHO – Low Back Pain Fact Sheet
https://www.who.int/news-room/fact-sheets/detail/low-back-pain - The Lancet Rheumatology – Global Burden of Low Back Pain
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(23)00098-X/fulltext - MidAmerica Orthopaedics – 4 Facts About Spinal Fusion
https://midamericaortho.com/blog/272-4-facts-about-spinal-fusion - Cleveland Clinic – Minimally Invasive Spine Surgery: Procedure, Risks & Benefits
https://my.clevelandclinic.org/health/treatments/17235-minimally-invasive-spine-surgery - SpineTogether – Understanding Minimally Invasive Spine Surgery
https://spinetogether.com/all-posts/minimally-invasive-spine-surgery